The cost-effectiveness of vaccination in the United States against human papillomavirus (HPV), a sexually-transmitted virus that causes cervical cancer, will be optimized by achieving universal vaccine coverage in young adolescent girls, by targeting initial “catch-up” efforts to vaccinate women younger than 21 years of age, and by revising current screening policies, according to an analysis by Harvard School of Public Health (HSPH).
In the U.S. in 2007, cervical cancer developed in more than 11,000 women and killed 3,600 women. Cervical cancer (cervical cancer vaccine)is caused by infection with high-risk “oncogenic” types of HPV, also associated with other cancers.
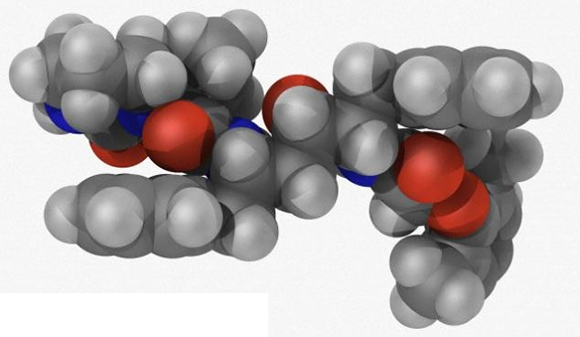
Worldwide, HPV types 16 (HPV-16) and 18 (HPV-18) cause approximately 70% of cervical cancer cases. Vaccines against HPV-16 and HPV-18 appear to be highly efficacious in preventing HPV-16 and HPV-18 infections and cervical disease in females who have not previously been infected with these types.
The quadrivalent vaccine currently licensed in the U.S. also prevents low-risk HPV types 6 and 11 (HPV-6 and HPV-11) infections, which are responsible for most genital warts and juvenile-onset recurrent respiratory papillomatosis (JORRP), a rare but severe respiratory condition usually diagnosed in infancy that may be related to a mother’s infection with genital warts.
Cervical cancer prevention in the U.S. has traditionally relied on a screening program involving frequent cytology (Pap smear) and/or HPV DNA testing, recommended annually or biennially for sexually-active women.
HPV vaccination raises questions regarding the age at which to vaccinate females, target groups for temporary catch-up programs, and appropriate changes to screening practices.
Read more at EurekAlert